Human Reproduction
Multiple Choice Questions (MCQs)
1. Choose the incorrect statement from the following
(a) in birds and mammals internal fertilisation takes place
(b) colostrum contains antibodies and nutrients
(c) polyspermy is prevented by the chemical changes in the egg surface
(d) in the human female implantation occurs almost seven days after fertilisation
Show Answer
Answer
(c) Polyspermy describes on egg that has been fertilised by more than one sperm. During fertilisation, binding of the sperm to the egg induces depolarisation of the egg plasma membrane that block the entry of additional sperms. Rest all statements are correct.

- (a) This statement is correct because in both birds and mammals, internal fertilisation does indeed take place.
- (b) This statement is correct because colostrum, the first form of milk produced by mammals immediately following delivery of the newborn, contains antibodies and nutrients essential for the newborn’s immune system and nutrition.
- (d) This statement is correct because in human females, implantation of the fertilised egg into the uterine wall typically occurs about seven days after fertilisation.
2. Identify the correct statement from the following.
(a) High levels of estrogen triggers the ovulatory surge.
(b) Oogonial cells start to proliferate and give rise to functional ova in regular cycles from puberty onwards.
(c) Sperms released from seminiferous tubules are poorly motile/ non-motile.
(d) Progesterone level is high during the post ovulatory phase of menstrual cycle.
Show Answer
Answer
(d) Post-ovulatory phase is also known as the luteal phase. During this period, the follicle proper folds inward on itself and transform into the corpus luteum which is a steroidogenic cluster of cells that produces estrogen and progesterone. The action of progesterone increases the basal body temperature. So, the correct answer is “Progesterone level is high during the post-ovulatory phase of the menstrual cycle.”
-
(a) High levels of estrogen do not directly trigger the ovulatory surge. Instead, it is the surge in luteinizing hormone (LH) that triggers ovulation. High levels of estrogen lead to a positive feedback mechanism that results in the LH surge.
-
(b) Oogonial cells do not start to proliferate and give rise to functional ova from puberty onwards. Oogenesis is largely completed before birth, and females are born with a finite number of oocytes. These oocytes are arrested in prophase I of meiosis and only resume development during each menstrual cycle after puberty.
-
(c) Sperms released from seminiferous tubules are not poorly motile/non-motile. They gain motility and the ability to fertilize an egg as they pass through the epididymis.
3. Spot the odd one out from the following structures with reference to the male reproductive system
(a) Rete testis
(b) Epididymis
(c) Vasa efferentia
(d) Isthmus
Show Answer
Answer
(d) Isthmus is the part of female reproductive system. The Fallopian tube (oviduct) in female reproductive system shows four regions, i.e., Infundibulum, ampulla, isthmus and uterine part. Isthmus has a narrow lumen and it joins the uterus. It is the line that demacrates the body of the uterus from the cervix.

Female reproductive system showing porition of isthmus

LS of testis showing rete testis, epididymis and vasa efferantia
-
Rete testis: This is a network of tubules located in the testis that carries sperm from the seminiferous tubules to the vasa efferentia. It is a part of the male reproductive system.
-
Epididymis: This is a long, coiled tube that stores and carries sperm from the testes. It is an essential part of the male reproductive system where sperm matures and gains motility.
-
Vasa efferentia: These are ducts that transport sperm from the rete testis to the epididymis. They are part of the male reproductive system and play a crucial role in the movement of sperm.
4. Seminal plasma, the fluid part of semen, is contributed by I. Seminal vesicle II. Prostate III. Urethra IV. Bulbourethral gland
(a) I and II
(b) I, II and IV
(c) II, III and IV
(d) I an IV
Show Answer
Answer
(b) The male accessory glands include paired seminal vesicles, a prostate and paired bulbourethral glands. Secretions of these glands constitute the seminal plasma which is rich in fructose, calcium and certain enzymes.
The secretions of bulbourethral glands also helps in the lubrication of the penis. Urethra is the duct that extends through the penis in male reproductive system and serve a comman passage for both sperm and urine. In female, urethra has no reproductive function.
-
Option (a) I and II: This option is incorrect because it excludes the bulbourethral gland, which also contributes to the seminal plasma.
-
Option (c) II, III and IV: This option is incorrect because it includes the urethra, which does not contribute to the seminal plasma. The urethra serves as a passage for both sperm and urine but does not produce any secretions.
-
Option (d) I and IV: This option is incorrect because it excludes the prostate, which is a significant contributor to the seminal plasma.
5. Spermiation is the process of the release of sperms from
(a) seminiferous tubules
(b) vas deferens
(c) epididymis
(d) prostate gland
Show Answer
Thinking Process
The fully developed sperms become free in the cavity of seminiferous tubules.
Answer
(a) The process of release of spermatozoa from Sertoli cells into the cavity of the seminiferous tubules is called spermiation. From here, sperms pass via vasa efferentia into the epididymis for temporary storage.
-
(b) Vas deferens: The vas deferens is a duct that transports mature sperm from the epididymis to the urethra in preparation for ejaculation. It is not involved in the initial release of sperms from the seminiferous tubules.
-
(c) Epididymis: The epididymis is a long, coiled tube where sperm mature and are stored temporarily. It is not the site of spermiation, which occurs in the seminiferous tubules.
-
(d) Prostate gland: The prostate gland is responsible for secreting a fluid that is a component of semen. It does not play a role in the release of sperms from the seminiferous tubules.
6. Mature Graafian follicle is generally present in the ovary of a healthy human female around
(a) 5-8 day of menstrual cycle
(b) 11-17 day of menstrual cycle
(c) 18-23 day of menstrual cycle
(d) 24-28 day of menstrual cycle
Show Answer
Thinking Process
The menstrual cycle can be divided into the following phases, i.e., menstrual phase, follicular (proliferating) phase, ovulatory phase and luteal phase.
Answer
(b) In humans (female), the menstrual cycle lasts for about 28/29 days. It is the follicular phase in which the primary follicles in the ovary grow to become a fully mature graafian follicle (due to FSH stimulation). This phase (follicular) lasts for about 14 days.
The secretion of gonadotropins ( $\mathrm{LH}$ and $\mathrm{FSH}$ ) increases gradually during this phase and stimulates secretion of estrogen by the growing follicles both LH and FSH attain a peak level in the middle of cycle (about 14th day).
This rapid secretion of $\mathrm{LH}$ called $\mathrm{LH}$ surge, induces rupture of Graafian follicle and thereby the release of ovum. This ovulatory phase is followed by the luteal phase during which the remaining follicular cells enlarge to become the corpus luteum.
-
(a) 5-8 day of menstrual cycle: During this period, the menstrual cycle is still in the early follicular phase. The primary follicles are just beginning to develop and have not yet matured into a Graafian follicle. The Graafian follicle typically matures closer to the middle of the cycle.
-
(c) 18-23 day of menstrual cycle: By this time, the ovulation phase has already occurred (around the 14th day), and the cycle has entered the luteal phase. The Graafian follicle has already ruptured to release the ovum, and the remaining follicular cells have transformed into the corpus luteum.
-
(d) 24-28 day of menstrual cycle: This period is also part of the luteal phase, where the corpus luteum is present. The Graafian follicle has already ruptured and released the ovum earlier in the cycle, so it is no longer present in its mature form.
7. Acrosomal reaction of the sperm occurs due to
(a) its contact with zona pellucida of the ova
(b) reactions within the uterine environment of the female
(c) reactions within the epididymal environment of the male
(d) androgens produced in the uterus
Show Answer
Thinking Process
The secondary oocyte reaching the Fallopian tube is surrounded by zona pellucida and corona radiata. A capacitated sperm passes through the corona radiata to reach the zona pellucida.
Answer
(a) One of the three glycoproteins (ZP3), functions as a sperm receptor and binds to a complementary molecule on the surface of the sperm head. Binding of the sperm head to the receptor molecule ZP3 induces the acrosome of the sperm to release its hydrolytic enzymes (sperm lysins).
The sperm lysins include
(i) Hyaluronidase, that hydrolyses hyaluronic acid of the follicular cells.
(ii) Corona penetrating enzyme dissolves corona radiata portion around the secondary oocyte by hydrolysing their ground substances.
(iii) Zona lysine or acrosin that helps to digest zona pellucida.
All these enzymes dissolve the corona radiata and zona pellucida and enable the sperm to reach the plasma membrane of the egg. The above changes in the head of sperm are called acrosome reaction.
-
(b) Reactions within the uterine environment of the female: The acrosomal reaction is specifically triggered by the interaction between the sperm and the zona pellucida of the ova, not by the general environment of the uterus.
-
(c) Reactions within the epididymal environment of the male: The epididymis is where sperm mature and are stored, but the acrosomal reaction occurs only when the sperm comes into contact with the zona pellucida of the ova, not within the male reproductive tract.
-
(d) Androgens produced in the uterus: Androgens are male sex hormones and are not involved in the acrosomal reaction. The acrosomal reaction is a response to the binding of the sperm to the zona pellucida of the ova, not influenced by hormones produced in the uterus.
8. Which one of the following is not a male accessory gland?
(a) Seminal vesicle
(b) Ampulla
(c) Prostate
(d) Bulbourethral gland
Show Answer
Thinking Process
The male accessory glands include paired seminal vesicles, a prostate and paired bulbourethral glands.
Answer
(b) Ampulla is one of the four region of Fallopian tubes. The oviducts (Fallopian tubes), uterus and vagina constitute the female accessory ducts. Each Fallopian tube is about 10-12 cm long and extends from the periphery of each ovary to the uterus.
The Fallopian tube shows four regions, i.e., infundibulum, ampulla, isthmus and uterine part. Ampulla region is the long, wide, thin walled part next to the infundibulum.
-
Seminal vesicle: The seminal vesicle is a male accessory gland that produces a significant portion of the fluid that becomes semen. This fluid contains proteins, enzymes, fructose, and other substances that support sperm viability and motility.
-
Prostate: The prostate gland is another male accessory gland that secretes a slightly alkaline fluid that forms part of the seminal fluid. This fluid helps to neutralize the acidity of the vaginal tract, prolonging the lifespan of sperm.
-
Bulbourethral gland: The bulbourethral glands, also known as Cowper’s glands, are male accessory glands that produce a pre-ejaculate fluid. This fluid helps to lubricate the urethra for sperm to pass through and neutralizes traces of acidic urine in the urethra.
9. The immature male germ cell undergo division to produce sperms by the process of spermatogenesis. Choose the correct one with reference to above.
(a) Spermatogonia have 46 chromosomes and always undergo meiotic cell division
(b) Primary spermatocytes divide by mitotic cell division
(c) Secondary spermatocytes have 23 chromosomes and undergo second meiotic division
(d) Spermatozoa are transformed into spermatids
Show Answer
Answer
(c) In testis, the immature male germ cells (spermatogonia) produce sperms by spermatogenesis. The spermatogonia present on the inside wall of seminiferous tubules multiply by mitotic division and increase in numbers.
Each spermatogonia is diploid and contains 46 chromosomes. $2 n$ Some of the spermatogonia called primary spermatocytes periodically undergo meiosis. A primary spermatocyte completes the first meiotic division (reduction division) leading to formation of two equal, haploid cells called secondary spermatocytes, which have only 23 chromosomes each $(n)$.
The secondary spermatocytes undergo the second phage of meiotic division to produce four equal, haploid spermatids. The spermatids are transformed into spermatozoa (sperms) by the process called spermiogenesis.
-
(a) Spermatogonia have 46 chromosomes and always undergo meiotic cell division: This statement is incorrect because spermatogonia undergo mitotic cell division to increase their numbers. Only some of the spermatogonia, called primary spermatocytes, undergo meiotic cell division.
-
(b) Primary spermatocytes divide by mitotic cell division: This statement is incorrect because primary spermatocytes undergo meiotic cell division, not mitotic. They undergo the first meiotic division to form secondary spermatocytes.
-
(d) Spermatozoa are transformed into spermatids: This statement is incorrect because spermatids are transformed into spermatozoa (sperms) through the process of spermiogenesis, not the other way around.
10. Match between the following representing parts of the sperm and their functions and choose the correct option.
| Column I | Column II | ||
|---|---|---|---|
| A. | Head | 1. | Enzymes |
| B. | Middle piece | 2. | Sperm motility |
| C. | Acrosome | 3. | Energy |
| D. | Tail | 4. | Genetic material |
Codes
| A | B | C | D | |
|---|---|---|---|---|
| (a) | 2 | 4 | 1 | 3 |
| (b) | 4 | 3 | 1 | 2 |
| (c) | 4 | 1 | 2 | 3 |
| (d) | 2 | 1 | 3 | 4 |
Show Answer
Answer
(b)
| Column I | Column II | |
|---|---|---|
| A. | Head | Genetic material |
| B. | Middle piece | Energy |
| C. | Acrosome | Enzymes |
| D. | Tail | Sperm motility |
The structure of a sperms composed of a head, neck, a middle piece and a tail. The sperm head contains an elongated haploid nucleus, the anterior portion of which is covered by a cap-like structure, acrosome. The acrosome is filled with enzymes that help in fertilisation of the ovum.
The middle piece possesses numerous mitochondria, which produce energy for the movement of tail that facilitate sperm motility essential for fertilisation.

Structure of a sperm
-
Option (a) is incorrect:
- A (Head) is matched with 2 (Sperm motility) instead of 4 (Genetic material).
- B (Middle piece) is matched with 4 (Genetic material) instead of 3 (Energy).
- D (Tail) is matched with 3 (Energy) instead of 2 (Sperm motility).
-
Option (c) is incorrect:
- B (Middle piece) is matched with 1 (Enzymes) instead of 3 (Energy).
- C (Acrosome) is matched with 2 (Sperm motility) instead of 1 (Enzymes).
- D (Tail) is matched with 3 (Energy) instead of 2 (Sperm motility).
-
Option (d) is incorrect:
- A (Head) is matched with 2 (Sperm motility) instead of 4 (Genetic material).
- B (Middle piece) is matched with 1 (Enzymes) instead of 3 (Energy).
- C (Acrosome) is matched with 3 (Energy) instead of 1 (Enzymes).
- D (Tail) is matched with 4 (Genetic material) instead of 2 (Sperm motility).
11. Which among the following has 23 chromosomes?
(a) Spermatogonia
(b) Zygote
(c) Secondary oocyte
(d) Oogonia
Show Answer
Answer
(c) Secondary oocyte has 23 chromosomes as it is a product of meiotic division of primary oocyte during oogenesis in the ovary. Oogenesis is initiated at the foetal ovary in the early embryonic stage of female and a fixed number of oogonia (gamete mother cells) are formed at before the birth of the female child no more oogonia are added after birth.
Spermatogonia is the immature male germ cells that produce sperms. Each spermatogonium is diploid (2n) and contain 46 chromosomes.
The haploid nucleus of the sperms and that of the ovum fuse together to form a diploid (2n) zygote i.e., 46 chromosomes.
During foetal development, certain cells in the germinal epithelium of the ovary undergo mitotic divisions, producing undifferentiated germ cells called oogonia. The oogonia is diploid (2n) and contains 46 chromosomes.
-
Spermatogonia: Spermatogonia are immature male germ cells that produce sperms. Each spermatogonium is diploid (2n) and contains 46 chromosomes, not 23.
-
Zygote: The zygote is formed by the fusion of the haploid nucleus of the sperm and the haploid nucleus of the ovum, resulting in a diploid (2n) cell with 46 chromosomes, not 23.
-
Oogonia: Oogonia are undifferentiated germ cells in the ovary that undergo mitotic divisions during fetal development. Each oogonium is diploid (2n) and contains 46 chromosomes, not 23.
12. Match the following and choose the correct options.
| Column I | Column II | |
|---|---|---|
| A. | Trophoblast | 1. Embedding of blastocyst in the endometrium |
| B. | Cleavage | 2. Group of cells that would differentiate as embryo |
| C. | Inn | 3. Outer layer of blastocyst attached to the endometrium |
| D. | Implantation | 4. Mitotic division of zygote |
Codes
| A | B | C | D | ||||
|---|---|---|---|---|---|---|---|
| (a) | 2 | 1 | 3 | 4 | |||
| (b) | 3 | 4 | 2 | 1 | |||
| (c) | 3 | 1 | 2 | 4 | |||
| (d) | 2 | 4 | 3 | 1 |
Show Answer
Answer
(b)
| Column I | Column II | |
|---|---|---|
| A. | Trophoblast | Outer layer of blastocyst attached to the endometrium |
| B. | Cleavage | Mitotic division of zygote |
| C. | Inner cell mass | Group of cell that would differentiate as embryo |
| D. | Implantation | Embedding of blastocyst in the endometrium |
-
Option (a) is incorrect because:
- A. Trophoblast is matched with “Group of cells that would differentiate as embryo” instead of “Outer layer of blastocyst attached to the endometrium”.
- B. Cleavage is matched with “Embedding of blastocyst in the endometrium” instead of “Mitotic division of zygote”.
- C. Inner cell mass is matched with “Outer layer of blastocyst attached to the endometrium” instead of “Group of cells that would differentiate as embryo”.
- D. Implantation is matched with “Mitotic division of zygote” instead of “Embedding of blastocyst in the endometrium”.
-
Option (c) is incorrect because:
- B. Cleavage is matched with “Embedding of blastocyst in the endometrium” instead of “Mitotic division of zygote”.
- C. Inner cell mass is matched with “Group of cells that would differentiate as embryo” instead of “Outer layer of blastocyst attached to the endometrium”.
- D. Implantation is matched with “Mitotic division of zygote” instead of “Embedding of blastocyst in the endometrium”.
-
Option (d) is incorrect because:
- A. Trophoblast is matched with “Group of cells that would differentiate as embryo” instead of “Outer layer of blastocyst attached to the endometrium”.
- C. Inner cell mass is matched with “Outer layer of blastocyst attached to the endometrium” instead of “Group of cells that would differentiate as embryo”.
13. Which of the following hormones is not secreted by human placenta?
(a) hCG
(b) Estrogens
(c) Progesterone
(d) $\mathrm{LH}$
Show Answer
Answer
(d) LH-Luteizing Hormone is produced by anterior pituitary gland. The placenta is an organ that connects the developing embryo (foetus) and maternal body (uterine wall) to allow nutrient uptake, waste elimination and gas exchange via the mother’s blood supply.
Placenta also acts as an endocrine tissue and produces several hormones like Human Chorionic Gonadotropin (hCG), Human Placental Lactogen (hPL), estrogens, progesterone, etc.
-
(a) hCG: Human Chorionic Gonadotropin (hCG) is indeed secreted by the human placenta. It supports the corpus luteum in the ovary to continue producing progesterone during the early stages of pregnancy.
-
(b) Estrogens: Estrogens are also secreted by the human placenta. They play a crucial role in maintaining the pregnancy and preparing the body for childbirth.
-
(c) Progesterone: Progesterone is another hormone secreted by the human placenta. It helps maintain the uterine lining for a successful pregnancy and prevents contractions in the early stages.
14. The vas deferens receives duct from the seminal vesicle and opens into urethra as
(a) epididymis
(b) ejaculatory duct
(c) efferent ductule
(d) ureter
Show Answer
Thinking Process
The male sex accessory ducts include rete testis, vasa efferentia, epididymis and vas deferens.
Answer
(b) The vas deferens is a continuation of the cauda epididymis (tail part of epididymis). It is about $40 \mathrm{~cm}$ long and slightly coiled at first but becomes straight as it enters the abdominal cavity through the inguinal canal.
Here, it passes over the urinary bladder, curves round the ureter and joins a duct from seminal vesicle and opens into urethra as the ejaculatory duct. These ducts store and transport the sperms from the testis to the outside through urethra.
-
(a) epididymis: The epididymis is a coiled tube located at the back of the testis where sperm is stored and matured. It does not receive a duct from the seminal vesicle nor does it open into the urethra.
-
(c) efferent ductule: The efferent ductules are small ducts that connect the rete testis to the head of the epididymis. They do not receive a duct from the seminal vesicle nor do they open into the urethra.
-
(d) ureter: The ureter is a tube that carries urine from the kidney to the urinary bladder. It is not involved in the transport of sperm and does not receive a duct from the seminal vesicle nor does it open into the urethra.
15. Urethral meatus refers to the
(a) urinogenital duct
(b) opening of vas deferens into urethra
(c) external opening of the urinogenital duct
(d) muscles surrounding the urinogenital duct
Show Answer
Answer
(c) The urethra originates from the urinary bladder and extends through the penis to its external opening called urethral meatus. Opening of vas deferens along with a duct of seminal vesicle open into urethra as the ejaculatory duct.
- (a) The urinogenital duct is a general term that can refer to the combined urinary and genital ducts, but it does not specifically refer to the external opening of the urethra, which is the urethral meatus.
- (b) The opening of the vas deferens into the urethra is known as the ejaculatory duct, not the urethral meatus.
- (d) The muscles surrounding the urinogenital duct are not referred to as the urethral meatus; they are part of the pelvic floor muscles and sphincters that control the flow of urine and semen.
16. Morula is a developmental stage
(a) between the zygote and blastocyst
(b) between the blastocyst and gastrula
(c) after the implantation
(d) between implantation and parturition
Show Answer
Answer
(a) The haploid nucleus of the sperms and that of the ovum fuse together to form a diploid zygote. As the zygote moves through the isthmus of the oviduct towards the uterus, the mitotic division (cleavage) starts and forms 2, 4, 8, 16 daughter cells called blastomeres.
The embryo with $8-16$ blastomeres is called a morula. The morula continues to divide and transforms into blastocyst as it moves further to get embedded in the endometrium of the uterus. This is called implantation.
-
(b) between the blastocyst and gastrula: This option is incorrect because the morula stage occurs before the blastocyst stage, not between the blastocyst and gastrula stages. The morula develops into the blastocyst, which then undergoes further development to form the gastrula.
-
(c) after the implantation: This option is incorrect because the morula stage occurs before implantation. The morula transforms into the blastocyst, which then implants into the endometrium of the uterus.
-
(d) between implantation and parturition: This option is incorrect because the morula stage occurs much earlier in the developmental process, before implantation. Parturition refers to the process of giving birth, which is the final stage of pregnancy, long after the morula stage.
17. The membranous cover of the ovum at ovulation is
(a) corona radiata
(b) zona radiata
(c) zona pellucida
(d) chorion
Show Answer
Answer
(a) The ovum is enclosed by the inner thin, transparent, non-cellular coat zona pellucida and outer thick coat corona radiata. During fertilisation sperm first comes in contact with the corona radiata and zona pellucida to reach the plasma membrane of the egg (ovum).
-
(b) zona radiata: This term is not commonly used in the context of the ovum’s membranous coverings. The correct term is “zona pellucida,” which is a specific glycoprotein layer surrounding the plasma membrane of mammalian oocytes.
-
(c) zona pellucida: While the zona pellucida is indeed a membranous cover of the ovum, it is not the outermost layer at ovulation. The outermost layer is the corona radiata, which surrounds the zona pellucida.
-
(d) chorion: The chorion is an extra-embryonic membrane that forms part of the placenta in mammals. It is not a membranous cover of the ovum at ovulation.
18. Identify the odd one from the following
(a) labia minora
(b) fimbriae
(c) infundibulum
(d) isthmus
Show Answer
Answer
(a) The female accessory ducts constitute the oviducts (Fallopian tubes), uterus and vagina. Each Fallopian tube extends from the periphery of each ovary to the uterus. The part closer to the ovary is the funnel-shaped infundibulum.
The edges of the infundibulum possess finger-like projections called fimbriae. The infundibulum leads to a wider part of the oviduct called ampulla. The last part of the oviduct is isthmus. While, labia minora is the female external genitalia.
-
Fimbriae: These are finger-like projections at the edge of the infundibulum, which is part of the female reproductive system’s oviducts (Fallopian tubes). They help in capturing the ovum released from the ovary.
-
Infundibulum: This is the funnel-shaped part of the Fallopian tube that is closest to the ovary. It plays a crucial role in guiding the ovum from the ovary into the Fallopian tube.
-
Isthmus: This is the narrow part of the Fallopian tube that connects the ampulla to the uterus. It is involved in the transport of the ovum or fertilized egg towards the uterus.
All these options (fimbriae, infundibulum, and isthmus) are parts of the female reproductive system’s oviducts (Fallopian tubes), whereas labia minora is part of the external genitalia.
Very Short Answer Type Questions
1. Given below are the events in human reproduction. Write them in correct sequential order.
Insemination, gemetogenesis, fertilisation, parturition, gestation, implanation.
Show Answer
Thinking Process
Humans reproduce sexually and give birth to young babies.
Answer
The reproductive events in humans include
(i) Gametogenesis Formation of gemetes (sperm in males, ova in females).
(ii) Insemination Transfer of sperm into female reproductive tract.
(iii) Fertilisation Fusion of male and female gemetes.
(iv) Implantation Formation, development and then attachment of blastocyst to the uterine wall.
(v) Gestation Embryonic development inside female body.
(vi) Parturition Delivery of the baby.
2. The path of sperm transport is given below. Provide the missing steps in blank boxes.

Show Answer
Answer

The seminiferous tubules of the testes open into the vasa efferentia through rete testis. The vasa efferentia leave the testes and open into epididymis located along the posterior surface of each testes. The epididymis leads to vas deferens that ascends to the abdomen and loops over the urinary bladder.
It receives a duct from seminal vesicle and opens into urethra as the ejaculatory duct. These ducts store and transport the sperms from the testes to the outside through urethra.
3. What is the role of cervix in the human female reproductive system?
Show Answer
Thinking Process
The uterus (womb) is a large, pyriform, highly elastic sac specialised for the development of the embryo. It shows four regions, fundus, body, isthmus and cervix.
Answer
(i) The fundus is the broad, curved, dome-shaped upper area that receives the Fallopian tubes.
(ii) The body is the main part of the uterus, that starts directly below the level of the Fallopian tubes and continues downward until the uterine walls and cavity begin to narrow.
(iii) The isthmus is the lower, narrow neck region.
(iv) The cervix is the lowest part that extends downward from the isthmus until it opens into the vagina.

Fertilisation arrested in metaphase
Implantation
4. Why are menstrual cycles absent during pregnancy?
Show Answer
Answer
The menstrual flow results due to breakdown of endometrial lining of the uterus and its blood vessels which forms liquid that comes out through vagina. Menstruation only occurs if the released ovum is not fertillised.
During pregnancy, all events of the menstrual cycle stop and the corpus luteum secretes large amounts of progesterone which is essential for the maintenance of the endometrium. These changes lead to no menstruation, during pregnancy.
Note Lack of menstruation may be indicative of pregnancy. However, it may also be caused due to some other underlying causes like stress, poor health, etc.
5. Female reproductive organs and associated functions are given below in column I and II. Fill the blank blanks.
| Column I | Column II |
|---|---|
| Ovaries | Ovulation |
| Oviduct | $A$ |
| $B$ | Pregnancy |
| Vagina | Birth |
Show Answer
Answer
| Column I | Column II |
|---|---|
| Ovaries | Ovulation |
| Oviduct | Fertilisation |
| Uterus | Pregnancy |
| Vagina | Birth |
The female reproductive system consists of a pair of ovaries, a pair of Fallopian tubes (oviducts), uterus, vagina, external genitalia and mammary glands.
The ovaries have both an exocrine function (production of ova) and an endocrine function (secretion) of female sex hormones.
The oviduct (Fallopian tube) conveys the egg from the ovary to the uterus, and also provides the appropriate environment for its fertilisation. The uterus (womb) is a large, inverted, pear-shaped, elastic sac specialised for the development of the embryo.
The vagina is adapted for receiving the penis during copulation, allowing menstrual flow and serving as the birth canal during parturition
6. From where the parturition signals arise-mother or foetus? Mention the main hormone involved in parturition.
Show Answer
Answer
Parturition is induced by a complex neuroendocrine mechanism. The signals for parturition originate from the fully developed foetus and the placenta which induce mild uterine contractions called foetal ejection reflex.
The hormone involved in parturition is oxytocin that acts on the uterine muscle and causes stronger uterine contractions. This leads to the expulsion of the baby out of the uterus through the birth canal.
7. What is the significance of epididymis in male fertility?
Show Answer
Answer
The epididymis helps the sperm in attaining maturity, acquiring increased motility and fertilising capacity. It also stores sperms for a short period before entering the vasa deferens. The epididymis shows peristatic and segmenting contractions at intervals to push the sperm away from the testis.
8. Give the names and functions of the hormones involved in the process of spermatogenesis. Write the names of the endocrine glands from where they are released.
Show Answer
Answer
Hormones involved in spermatogenesis are
| Hormone | Function | Gland |
|---|---|---|
| Gonadotrophin releasing hormone $(G n R H)$ |
Acts on pituitary to secrete LH and FSH. | Hypothalamus |
| Luteinizing Hormone (LH) | Acts on Leydig cells and stimulates synthesis and secretion of androgens |
Pituitary |
| Androgens | Stimulate process of spermatogenesis | Testis |
| Follicle Stimulating Hormone (FSH) |
Acts ons sertoli cell and stimulates secretion of some factors that help in process of spermiogenesis |
Pituitary |
9. The mother germ cells are transformed into a mature follicle through series of steps. Provide the missing steps in the blank boxes.

Show Answer
Answer
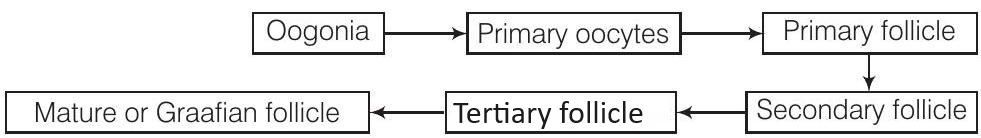
The germinal epithelial cells divide repeatedly until many diploid oogonia are formed. The oogonia grow to form primary oocytes. Each primary oocyte then gets surrounded by a layer of granulosa cells and then called the primary follicle. The primary follicles get surrounded by more layers of granulosa cells and called secondary follicles.
The secondary follicle soon transforms into a tertiary follicle which is characterised by a fluid filled cavity called antrum. The primary oocyte within the tertiary follicle undergoes meiotic division to become a secondary oocyte and a first polar body (haploid).
The tertiary follicle further changes into the mature follicle or Graafian follicle. The Graafian follicle now ruptures to release the secondary oocyte (ovum) from the ovary by the process called ovulation
10. During reproduction, the chromosome number (2n) reduces to half $(n)$ in the gametes and again the original number $(2 n)$ is restored in the offspring. What are the processes through which these events take place?
Show Answer
Thinking Process
Gametes are haploid while zygotes are diploid.
Answer
The meiotic cell division reducers the chromosome numbers to half during gametogenesis and diploid (2n) number of chromosome is restored by the union of male and female gamete through process of fertilisation.
11. What is the difference between a primary oocyte and a secondary oocyte?
Show Answer
Answer
Primary oocyte is a diploid cell formed in foetal ovary when the gamete mother cell, oogonia is arrested at prophase-l of meiosis. Secondary oocyte is the haploid cell formed from primary oocyte that completes its first meiotic division, during puberty and produces the female gamete ova( $(n)$.
12. What is the significance of ampullary-isthmic junction in the female reproductive tract?
Show Answer
Answer
The act of fertilisation takes place in the female genital track that is at the junction of the isthmus and ampulla (ampullary - isthmic junction) of the Fallopian tube.
Note Fertilisation can only occur if the ovum and sperms are transported simultaneously to the ampullary - isthmic junction. All copulations do not lead to fertilisation and pregnancy.
13. How does zona pellucida of ovum help in preventing polyspermy?
Show Answer
Answer
When a sperm penetrates ovum, it induces changes in the membrane that make the zona pellucida layer impenetrable to additional sperms. Thus, it ensures that only one sperm can fertilise an ovum and stops polyspermy.
14. Mention the importance of $\mathrm{LH}$ surge during menstrual cycle.
Show Answer
Answer
Rapid secretion of $\mathrm{LH}$ leading to its maximum level during the mid menstrual cycle (14th day) called LH surge induces rupture of Graafian follicle and thereby the release of ovum (ovulation).
The ovulation (ovulatory phase) is followed by the luteal phase during which the remaining parts of the Graafian follicle transform as the corpus luteum. The corpus luteum secretes large amounts of progesterone which is essential for maintenance of the endometrium. Such an endometrium is necessary of implantation of the fertilised ovum and other events of pregnancy.
15. Which type of cell division forms spermatids from the secondary spermatocytes?
Show Answer
Answer
The secondary spermatocytes undergo the second meiotic division to produce four equal, haploid spermatids.
Note Secondary spermatocytes are produced, when the primary spermatocytes undergo the first meiotic division (reduction division).
Short Answer Type Questions
1. A human female experiences two major changes, menarche and menopause during her life. Mention the significance of both the events.
Show Answer
Answer
In human beings, initiation of menstruation at puberty (between age 9-15 years) is called menarche. While, menstrual cycles ceases around 50 years of age, that is termed as menopause. Menarche signifies the maturation and readiness of the female reproductive system for child bearing.
It marks the capability of the ovaries to produce mature oocyte (female gamete) that can now be fertilised by the sperm and also that the uterus is capable of supporting the foetal growth and development.
Menopause signifies the end of child bearing age. At this age supply of healthy eggs is very low, the levels of the hormones secreted by the ovaries decline and the menstruation stops. The uterus no longer remains conductive for foetal growth.
2. (a) How many spermatozoa are formed from one secondary spermatocyte?
(b) Where does the first cleavage division of zygote take place?
Show Answer
Thinking Process
In testis, the spermatogonia (immature germ cells) present in the form of germinal layer on the inner wall of seminiferous tubules multiply by mitotic division and increase in numbers. Each spermatogonium is diploid and contains 46 chromosomes. Some of them periodically undergo meiosis and are called primary spermatocytes.
Answer
(a) A primary spermatocyte completes the first meiotic division (reduction division) leading to formation of two equal, haploid cells called secondary spermatocytes $(n=23$ chromosomes each). The secondary spermatocytes undergo the second meiotic division to produce four equal, haploid spermatids (n)., each spermatids produce spermatazoa.
(b) The mitotic division called cleavage starts $30 \mathrm{~h}$ after fertilisation when as to the zygote moves through the isthmus the Fallopian tube (oviduct) towards the uterus and forms blastomeres.
3. Corpus luteum in pregnancy has a long life. However, if fertilisation does not take place, it remains active only for 10-12 days. Explain.
Show Answer
Answer
The ruptured Graafian follicle transform into the corpus luteum and secretes large amounts of progesterone which is essential for the maintenance of the endometrium. Such an endometrium is required for the implantation of fertilised ovum (blastocyst) and other events of pregnancy.
That’s why corpus luteum in pregnancy has a long life. But in the absence of fertilisation, maintenance of endometrium is not required. Therefore, corpus luteum degenerates with in 10-12 days.
4. What is foetal ejection reflex? Explain how it leads to parturition?
Show Answer
Answer
Foetal ejection reflex encompasses the mild uterine contractions in response to the signals that originate from the fully developed foetus and the placenta. This triggers release of oxytocin from maternal pituitary. Oxytocin acts on the uterine muscle and causes stronger contractions, which in turn stimulates further secretion of oxytocin.
The stimulatory reflex between the uterine contraction and oxytocin secretion continues resulting in stronger and stronger contractions leading to the expulsion of baby out of uterus through birth canal.
5. Except endocrine function, what are the other functions of placenta.
Show Answer
Answer
Placenta is structural and functional unit between developing embryo (foetus) and maternal body.
Placenta acts as an endocrine tissue and produces several hormones like human Chorionic Gonadotropin (hCG), human Placental Lactogen (hPL), estrogens, progesterones, etc.
Other than the endocrine function, placenta also facilitates the supply of oxygen and nutrients to the embryo and removes carbon dioxide and excretory/waste materials produced by the developing faetus.
6. Why doctors recommend breast feeding during initial period of infant growth?
Show Answer
Answer
The milk produced during the initial few days of lactation is called colostrum which contains several antibodies (especially $1 \mathrm{gA}$ ) essential to develop resistance in the new-born babies against diseases. Breast-feeding during the initial period of infant growth is recommended by doctors for bringing up a healthy baby.
7. What are the events that take place in the ovary and uterus during follicular phase of the menstrual cycle.
Show Answer
Answer
The major events of the menstrual cycle are menstrual phase, follicular phase, ovulatory phase and luteal phase.
The follicular phase follows the menstrual phase. During this phase, the primary follicles in the ovary grow to become a fully mature Graafian follicle and simultaneously the endometrium of uterus regenerates through proliferation. These changes in the ovary and the uterus are induced by changes in the levels of pituitary and ovarian hormones.
The secretion of gonadotropins (LH and FSH) increases gradually during the follicular phase and stimulates follicular development as well as secretion of estrogens by the growing follicles.
Both LH and FSH attain a peak level in the middle of cycle (about 14th day). This rapid secretion of LH leading to its maximum level induces rupture of Graafian follicle to release ovum.
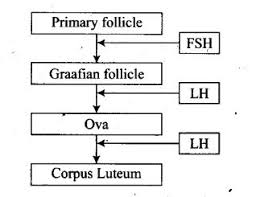
8. Given below is a flow chart showing ovarian changes during menstrual cycle. Fill in the spaces giving the name of the hormones responsible for the events shown.

Show Answer
Answer
The secretion of gonadotropins ( $\mathrm{LH}$ and $\mathrm{FSH}$ ) increases gradually during the follicular phase and stimulates follicular development as well as secretion of estrogens. Rapid secretion of LH leading to its maximum level during the midcycle (14th day) of menstrual cycle induces rupture of Graafian follicle to release ovum.
The remaining parts of the Graafian follicle transform into the corpus luteum. The corpus luteum secretes large amounts of progesterone which is essential for maintenance of the endometrium during pregnancy.
9. Give a schematic labelled diagram to represent oogenesis (without descriptions).
Show Answer
Answer

Schematic representation of oogenesis
10. What are the changes in the oogonia during the transition of a primary follicle to Graafian follicle?
Show Answer
Answer
The germinal epithelial cells divide repeatedly until many diploid oogonia are formed. The oogonia grow to form primary oocytes. Each primary oocyte then gets surrounded by a layer of granulosa cells and then called the primary follicle.
The primary follicles get surrounded by more layers of granulosa cells and called secondary follicles. The secondary follicle soon transforms into a tertiary follicle which is characterised by a fluid filled cavity called antrum.
The primary oocyte within the tertiary follicle undergoes meiotic division to become a secondary oocyte and a first polar body (haploid). The tertiary follicle further changes into the mature follicle or Graafian follicle that ruptures to release the secondary oocyte (ovum) from the ovary by the process called ovulation.
Long Answer Type Questions
1. What role does pituitary gonadotropins play during follicular and ovulatory phases of menstrual cycle? Explain the shifts in steroidal secretions.
Show Answer
Thinking Process
The major events of the menstrual cycle include menstrual phase, follicular phase, ovulatory phase and luteal phase.
Answer
Menstrual Phase (1-5 days)
Endrometrium breaks down the cell of endometrium secretions unfertilised ovum constitute menstrual flow. Progesteron production is reduced
Follicular Phese ( $6-13$ days)
Endometrium rebuilds, $\mathrm{FSH}$ and oestrogen secretion is increased.
Ovulatory Phase (14-16 days)
Both LH and FSH attain peak level. Estrogen level is also high. It leads to ovulation.
Luteal Phase (16-28 days)
In absence of fertilisation corpus luteum secretes progesterone. Endometrium Thickens and uterine glands become secretary.
The menstrual cycle starts with the menstrual phase, when menstrual flow occurs and it lasts for 3-5 days. It results due to breakdown of endometrial lining of the uterus and its blood vessels.
Follicular Phase The menstrual phase is followed by the follicular phase.
During this phase, the primary follicles in the ovary grow to become a fully mature Graafian follicle and simultaneously the endometrium of uterus regenerates through proliferation. These changes in the ovary and the uterus are induced by changes in the levels of pituitary and ovarian hormones.

Diagrammatic presentation of various events during a mentrual cycle
The secretion of gonadotropins (LH and FSH) increases gradually during the follicular phase and stimulates follicular development as well as secretion of estrogens by the growing follicles. Both LH and FSH attain a peak level in the middle of cycle (about 14th day).
Rapid secretion of $\mathrm{LH}$ leading to its maximum level during the mid-cycle called $\mathrm{LH}$ surge induces rupture of Graafian follicle and thereby the release of ovum (ovulation). The ovulation (ovulatory phase) is followed by the luteal phase during which the remaining parts of the Graafian follicle transform as the corpus luteum. The corpus luteum secretes large amounts of progesterone which is essential for maintenance of the endometrium.
Such an endometrium is necessary for implantation of the fertilised ovum and other events of pregnancy. In the absence of fertilisation, the corpus luteum degenerates.
This causes disintegration of the endometrium leading to menstruation.
2. Meiotic division during oogenesis is different from that in spermatogenesis. Explain how and why?
Show Answer
Answer
Oogenesis is different from that of spermatogenesis in the following aspects
| Spermatogenesis | Oogenesis |
|---|---|
| Sperm generation starts at puberty. | Oocytes generated before birth. |
| Many millions generated at a time. | Only one matures at a time, every month. |
| After two complete meiotic divisions, four equal sized cells produced. |
Meiosis-l get arrested at prophase-I and when completed at later stage, one big cell with almost all the cytoplasmand three very small sized cells produced. |
| They mature into flagellated and motile cell. | Mature ovum is non-flagellated and non-motile. |

Schematic representation of (a) Spermatogenesis (b) Oogenesis
Reasons
(i) Unequal cell division makes the ovum much larger than the other three polar bodies. Because ovum has more cytoplasm and more organelles, it has a better chance of surviving.
(ii) The male makes millions of tiny sperms while, the female makes only one egg per month that also waits for second meiotic division, until just before fertilisation. This is a way of conserving energy.
(iii) Sperm is smaller and motile as it has to move out of male system to female reproductive system. Larger egg has abundant reserve food so that embryo starts developing right after fertilisation.
3. The zygote passes through several developmental stages till implantation. Describe each stage briefly with suitable diagrams.
Show Answer
Thinking Process
The zygote undergoes mitotic division (cleavage) as it moves through isthmus of oviduct towards uterus and forms 2, 4, 8, 16 daughter cells called blastomeres.
Answer
The zygote passes through the following stages till implantations
(i) The embryo with 8-16 blastomeres is called a morula.
(ii) The morula continues to divide and transforms into blastocyst as it moves further into uterus.
(iii) The blastomeres in the blastocyst are arranged into a surface layer called trophoblast and a cluster of interior cells attached to trophoblast are called the inner cell mass.
(iv) The trophoblast layer then gets attached to the endometrium and inner mass cells get differentiated as embryo.
(v) After attachment, the uterine cells divide rapidly to cover the blastocyst.
(vi) The blastocyst becomes embedded in the uterine endometrium. This is called implantation.

Transport of ovum, fertilisation and passage of growing embryo through Fallopian tube
4. Draw a neat diagram of the female reproductive system and label the parts associated with the following (a) production of gamete, (b) site of fertilisation (c) site of implantation and (d) birth canal.
Show Answer
Answer
The female reproductive system consists of a pair of ovaries along with a pair of oviducts, uterus, cervix, vagina and the external genitalia located in pelvic region.
These parts are integrated structurally and functionally to support the processes of ovulation, fertilisation, pregnancy and birth.

Diagrammatic sectional view of the female reproductive system
Labels
(i) Ovary (production of gamete)
(ii) Isthmus-ampullary junction(site of fertilisation)
(iii) Uterine endometrium (site of implantation)
(iv) Cervix and vagina (birth canal)
5. With a suitable diagram, describe the organisation of mammary gland.
Show Answer
Answer
The description of mammary gland is as follows
(i) The mammary glands are paired structures (breasts) that contain undeveloped duct system and adipose tissue (fat containing cells).
(ii) During pregnancy, in response to oestrogen and progesterone, a glandular system develops for milk production.
(iii) Glandular tissue of each breast develops mammary lobes containing clusters of cells called alveoli.
(iv) The cells of alveoli secrete milk, which is stored in the cavities (lumens) of alveoli
(v) The alveoli open into mammary tubules. The tubules of each lobe join to form a mammary duct.
(vi) Several mammary ducts join to form a wider mammary ampulla which is connected to lactiferous duct through which milk is sucked out by the baby.

A diagrammatic sectional view of mammary gland